Nature has a peculiar way of offering solutions to human problems, sometimes from the most unexpected sources. In the vast repertoire of natural compounds, venoms are typically viewed as deadly weapons that animals use for hunting or defense. Yet, the story of how a potentially lethal venom accidentally became a lifesaving treatment represents one of medicine’s most remarkable serendipitous discoveries. This narrative of unexpected redemption—where a substance designed to kill instead preserved life—illuminates the complex relationship between humans and the natural world and demonstrates how scientific advancement often treads unpredictable paths.
The Unexpected Patient Zero

Our story begins with an unfortunate incident that would ultimately change medical history. In the late 1960s, a Brazilian farmer was working in his fields when he was bitten by a pit viper, specifically the jararaca snake (Bothrops jararaca). Rather than seeking immediate medical attention, the man noticed something peculiar in the aftermath of his envenomation. His chronic high blood pressure, which had troubled him for years, suddenly improved significantly. This bizarre observation—made by a victim rather than a scientist—sparked curiosity in the medical community. The farmer’s misfortune became the first documented case of snake venom inadvertently treating a human medical condition, setting in motion a scientific investigation that would eventually save millions of lives worldwide.
Understanding the Deadly Jararaca

The jararaca snake is a formidable predator native to southeastern Brazil, northern Argentina, and Paraguay. Growing up to 6 feet in length, this pit viper possesses a complex venom designed to immobilize prey and begin the digestive process before consumption. Its bite typically causes severe local pain, tissue damage, and systemic effects including hemorrhage, kidney failure, and a dramatic drop in blood pressure. The latter effect—hypotension—occurs because the venom contains peptides that inhibit the body’s angiotensin-converting enzyme (ACE), which normally helps maintain blood pressure. This particular mechanism initially evolved to help the snake subdue its prey by inducing circulatory shock, would ironically become the foundation for one of medicine’s most important discoveries in cardiovascular treatment.
The Scientific Detective Work

Following the farmer’s unusual report, Brazilian scientist Sérgio Ferreira began investigating the components of jararaca venom at his laboratory in São Paulo. Through meticulous biochemical analysis, Ferreira isolated peptides that specifically affected blood pressure regulation. His groundbreaking work identified small protein fragments that inhibited ACE, a key enzyme in the renin-angiotensin-aldosterone system that regulates blood pressure and fluid balance. These bradykinin-potentiating peptides (BPPs), as they were called, prevented the production of angiotensin II, a powerful vasoconstrictor that raises blood pressure. Ferreira’s findings caught the attention of scientists worldwide, including researchers at the pharmaceutical company Squibb (now Bristol-Myers Squibb), who recognized the potential medical applications of this venom component.
From Venom to Medication: The Birth of Captopril

The journey from toxic snake venom to pharmaceutical breakthrough required the expertise of medicinal chemist David Cushman and his colleague Miguel Ondetti at Squibb Laboratories. Using Ferreira’s research as a foundation, they worked to develop a synthetic molecule that could mimic the ACE-inhibiting properties of the venom peptides while being stable enough to function as an oral medication. After years of trial and error, in 1975 they successfully created captopril, the first oral ACE inhibitor drug. This revolutionary medication worked by binding to the same site on the ACE enzyme as the snake venom peptides, effectively preventing the formation of angiotensin II and thus lowering blood pressure. Captopril represented not just a new drug but an entirely new class of medications that would transform the treatment of hypertension and heart failure.
The Regulatory Hurdles and Early Skepticism
Despite its promising mechanism, captopril faced significant skepticism from the medical community and regulatory obstacles before reaching patients. Many physicians were wary of a medication derived from snake venom, concerned about potential toxic effects or unpredictable outcomes. The early clinical trials revealed side effects including skin rash, loss of taste, and proteinuria in some patients, causing further hesitation. Additionally, pharmaceutical executives questioned the market viability of a drug targeting hypertension, which at the time was not widely recognized as requiring aggressive treatment. Nonetheless, Squibb persisted through the FDA approval process, believing in captopril’s potential to address a significant unmet medical need.
The Clinical Breakthrough

In 1981, after extensive clinical trials demonstrating both safety and efficacy, captopril received FDA approval for treating hypertension. The medication quickly proved its worth in managing not just routine high blood pressure but also severe and treatment-resistant cases. Physicians soon discovered that captopril was particularly valuable for patients with heart failure, a condition where the heart cannot pump blood efficiently. By reducing the workload on the heart through lowering blood pressure and decreasing fluid retention, captopril significantly improved outcomes for heart failure patients. This expanded use represented a paradigm shift in cardiovascular treatment, as prior to ACE inhibitors, options for heart failure management were extremely limited and often ineffective.
Expanding the ACE Inhibitor Family

The success of captopril spawned the development of an entire class of medications based on the same mechanism. Pharmaceutical companies worldwide began creating new ACE inhibitors with improved properties, including longer duration of action allowing for once-daily dosing and fewer side effects. Medications like enalapril, lisinopril, ramipril, and benazepril expanded the therapeutic options for patients with cardiovascular conditions. These second-generation ACE inhibitors maintained the core mechanism of blocking angiotensin II production but offered advantages in terms of convenience and tolerability. Today, ACE inhibitors remain a cornerstone of treatment for hypertension, heart failure, and kidney protection in diabetes, with millions of prescriptions written annually.
Lives Saved and Quality of Life Improved

The impact of ACE inhibitors on public health has been nothing short of extraordinary. Before their development, hypertension often progressed unchecked, leading to heart attacks, strokes, and kidney failure. Heart failure patients faced grim prognoses with five-year survival rates worse than many cancers. The introduction of ACE inhibitors dramatically altered these outcomes. Studies have shown that these medications reduce the risk of stroke by approximately 30%, heart attacks by 20%, and heart failure mortality by up to 40%. Beyond mere survival statistics, ACE inhibitors have improved the quality of life for countless patients by reducing hospitalizations, preventing disability from cardiovascular events, and allowing people with chronic conditions to lead more normal lives.
Beyond Cardiovascular Disease: Unexpected Benefits

As ACE inhibitors became widely used, researchers discovered benefits extending beyond their original cardiovascular applications. These medications demonstrated remarkable kidney-protective effects, particularly in patients with diabetes, significantly slowing the progression of diabetic nephropathy. Some studies suggested potential neuroprotective benefits, reducing the risk of certain types of dementia and cognitive decline. Research also indicated possible benefits in preventing the progression of certain eye diseases related to diabetes and hypertension. Perhaps most surprisingly, during the COVID-19 pandemic, some data suggested that patients taking ACE inhibitors might have better outcomes if infected with the virus, though this remains an area of ongoing research.
The Economic Impact of a Venom-Inspired Medication
The economic implications of the ACE inhibitor discovery extend far beyond pharmaceutical profits. By preventing costly cardiovascular events like heart attacks, strokes, and heart failure hospitalizations, these medications have saved healthcare systems worldwide billions of dollars. A 2018 analysis estimated that ACE inhibitor therapy prevents approximately 86,000 premature deaths and 447,000 hospitalizations annually in the United States alone. Additionally, by helping working-age adults maintain their health, these medications have preserved workforce productivity and reduced disability payments. The return on investment from the initial research into snake venom has been astronomical, representing one of medicine’s most cost-effective developments.
The Ecological Irony: Conservation Implications
The jararaca snake’s contribution to medicine presents a powerful argument for biodiversity conservation. This species, once viewed primarily as a dangerous pest in its native range, gained new appreciation after its venom revolutionized cardiovascular treatment. The captopril story has become a textbook example of why preserving biodiversity matters—we simply don’t know which species might hold the next medical breakthrough. Conservation organizations now frequently cite the jararaca as evidence that even feared creatures may provide invaluable benefits to humanity. Ironically, a creature many humans would instinctively kill has saved more human lives than it could ever threaten, demonstrating the complex interdependence between human health and ecosystem preservation.
The Legacy of Serendipity in Medical Discovery

The captopril story exemplifies the crucial role of chance observations and serendipity in scientific advancement. Had that Brazilian farmer not noticed the change in his blood pressure after the snakebite, or had he not reported it to medical professionals, this discovery might have been delayed by decades or missed entirely. This case joins other famous serendipitous medical discoveries like penicillin, Viagra, and X-rays—all found while scientists were looking for something else entirely. Modern pharmaceutical research, with its highly targeted approaches and computational drug design, still cannot fully replace the value of unexpected observations and connections. The captopril discovery reminds us that keeping an open mind to unusual patterns and reports, even from non-scientists, remains essential to medical progress.
Future Frontiers: Venom-Based Medicine Today
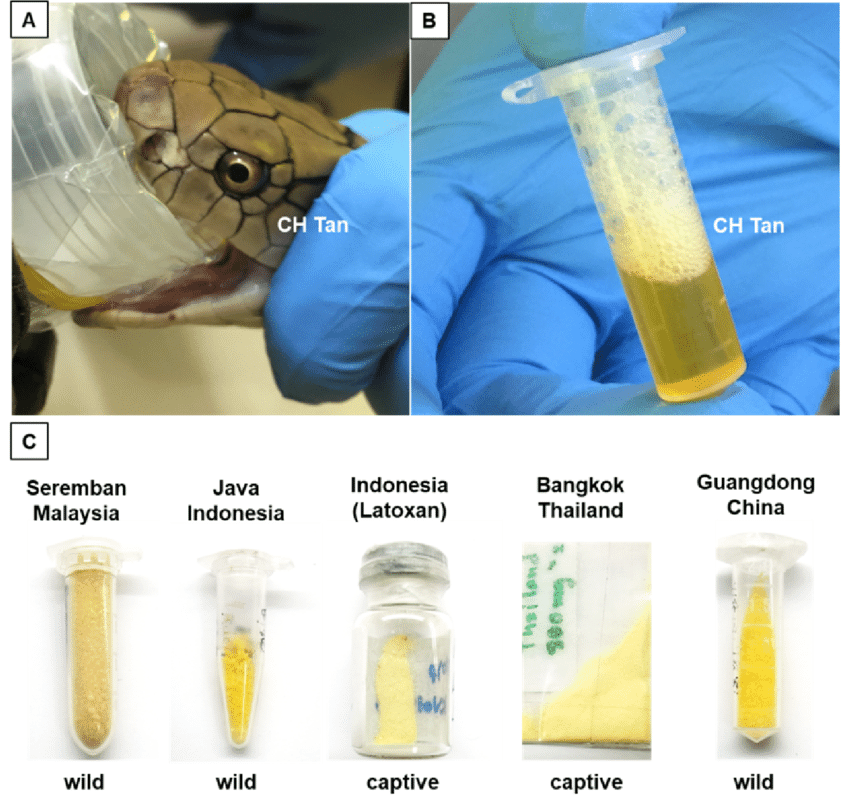
The success of captopril has inspired an entire field of research dedicated to exploring animal venoms for medical applications. Scientists are currently investigating compounds from spiders, scorpions, cone snails, and other snake venoms for potential treatments ranging from chronic pain to cancer. Ziconotide, derived from cone snail venom, is already approved for treating severe chronic pain resistant to other treatments. Researchers have identified a peptide from tarantula venom that shows promise in treating muscular dystrophy. Compounds from scorpion venom are being developed as potential treatments for autoimmune diseases and certain cancers. These ongoing investigations suggest that the captopril story may be just the first chapter in humanity’s utilization of venoms as a source of life-saving medicines.
The captopril story represents a profound irony—a substance evolved to kill transformed into one that saves lives. From a chance observation by a snake-bitten farmer to a medication that has helped hundreds of millions of people worldwide, this narrative exemplifies both the unexpected connections in nature and the power of scientific investigation to harness those connections for human benefit. The journey from venom to vital medication reminds us that solutions to our most pressing medical challenges may come from the most unlikely sources. As we continue to face new health threats, the lesson of captopril suggests that we should look not just to cutting-edge technology but also to the natural world—even its most feared aspects—for inspiration and answers. In the case of the jararaca snake and captopril, what began as a mistake ultimately became one of medicine’s greatest successes.




